HIPAA-covered entities must observe and respect their patient's right to access. Complying with HIPAA is the law.
HIPAA Right of Access
Imagine a patient urgently needing her medical records to make informed decisions about her treatment. She submits a request, expecting timely access, but encounters delays and obstacles. This scenario not only hinders patient care but also violates federal law. The HIPAA Right to Access is a fundamental provision for patients, granting them prompt access to their health information. Despite its importance, many healthcare providers inadvertently overlook critical aspects of this regulation, leading to costly penalties and eroded trust.
Recently, a mental health center faced a substantial $100,000 fine for failing to provide timely access to a patient's records. This case highlights common misconceptions and underscores the serious consequences of non-compliance. In this guide, we'll explore the intricacies of HIPAA's Right to Access, debunk prevalent myths, delve into often-overlooked implications, and provide actionable steps to ensure your organization remains compliant.
Case Study on Why HIPAA Right of Access Matter
A recent enforcement action highlights the need to address non-compliance and correct the issue quickly.
📍 What's the Outcome?
📍 Enforcement Action: The Office for Civil Rights (OCR) imposed a $100,000 civil monetary penalty on a mental health center for failing to comply with HIPAA's Right to Access provision.
📍 Key Findings: The center's operational challenges due to the COVID-19 pandemic were not accepted as valid reasons for non-compliance. OCR emphasized that patient rights remain a priority, regardless of external circumstances.
🔎 What Happened?
🔎 Patient Request: On March 18, 2020, a patient submitted a written request to access her medical records from the community mental health center.
🔎 Delayed Response: Despite multiple follow-up attempts, the patient did not receive her records in a timely manner. The records were provided 216 days after the initial request, well beyond the maximum allowable 60-day period (including the permissible extension).
🔎 Complaint Filed: Frustrated by the delay, the patient filed a complaint with the Office for Civil Rights (OCR).
⚙️ Lessons Learned?
⚙️ Compliance Is Non-Negotiable: Operational difficulties do not exempt providers from their obligations under HIPAA. When an incident occurs and is discovered, the organization's goal is to correct it.
⚙️ Importance of proactive measures: Having contingency plans and efficient systems is crucial to ensure compliance, even during emergencies.
⚙️ Potential for significant penalties: Financial consequences for non-compliance can be substantial.
- If the law allowed it, the regulators would ask for more: Observe how the OCR attempted to penalize the mental health center for the highest amount possible (i.e., the dollar $ amount partly calculated by the days left unresolved). However, the current law restricts the enforcement agency with an annual cap on that penalty. For more detailed information, read the HHS Notice of Proposed Determination.
What is the HIPAA Right to Access?
The Health Insurance Portability and Accountability Act (HIPAA) grants individuals the right to access their Protected Health Information (PHI) held by covered entities, such as healthcare providers, health plans, and healthcare clearinghouses.
The Right to Access (45 CFR § 164.524)
Key Provisions
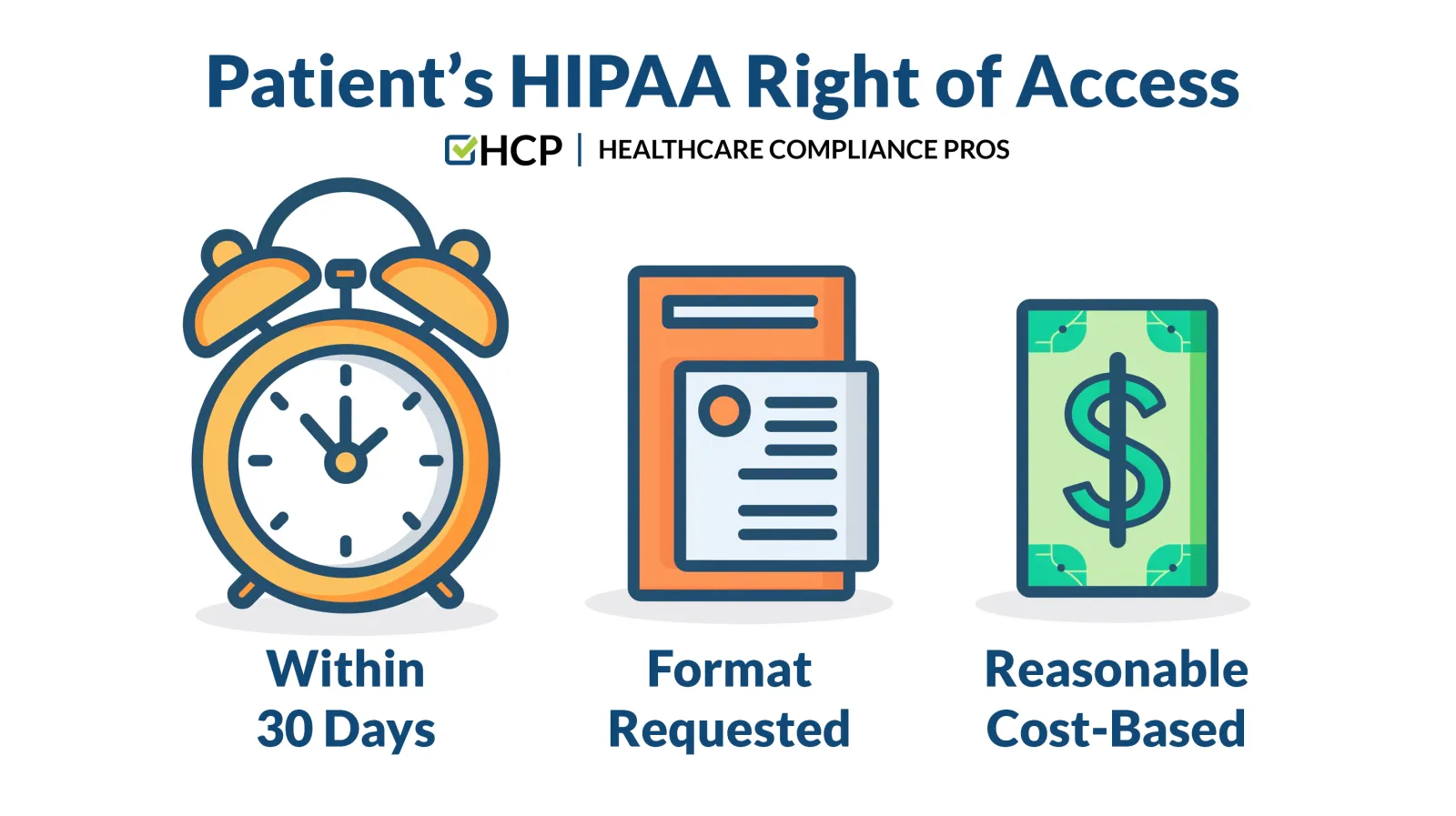
1. Timely Access.
Covered entities must provide access to PHI within 30 days of receiving a request. A one-time extension of an additional 30 days is permissible, but only with a written explanation to the individual outlining the reasons for the delay and the expected completion date.
2. Form and Format.
Individuals have the right to receive their PHI in the form and format they request if it is readily producible. This includes electronic copies if the PHI is maintained electronically. If the requested format is not readily producible, the information must be provided in a readable hard copy or other agreed-upon format.
3. Reasonable, Cost-Based Fees.
Providers may charge a reasonable fee that covers only the cost of:
- Labor for copying the PHI.
- Supplies for creating the paper copy or electronic media.
- Postage, if the individual requests the information mailed.
Fees cannot include costs associated with verifying, documenting, searching for, or retrieving the PHI.
4. Limited Grounds for Denial.
Access can only be denied in certain circumstances, such as when releasing the information could endanger the life or physical safety of the individual or another person. Even when denying access, providers must:
- Give a written denial explaining the basis for the denial.
- Inform the individual of their right to have the decision reviewed and how to file a complaint.
Debunking Common Myths About the Right to Access

Misunderstandings surrounding HIPAA's Right to Access can lead to inadvertent violations, putting healthcare providers at risk of substantial penalties and eroding patient trust. Let's pose some prevalent myths as questions and provide factual corrections to clarify these misconceptions.
❌ Myth 1: Providers Can Delay Access Due to Operational Challenges
✅ Question #1: Is it acceptable to delay providing records if we're experiencing staff shortages or high volumes of requests?
✅ Correction #1: No. HIPAA mandates timely access regardless of operational challenges. Providers must have processes to comply with access requirements, even during busy periods or unforeseen circumstances like the COVID-19 pandemic. Failure to do so is not considered a valid excuse and can result in penalties.
❌ Myth 2: Covered Entities Can Charge Higher Fees to Cover Administrative Costs
✅ Question #2: Can we include costs like retrieving, handling, or processing records in the fees we charge patients?
✅ Correction #2: No. Fees must be reasonable and strictly cost-based, limited to the actual costs of copying (labor and supplies) and postage if applicable. Charging for administrative tasks such as retrieval, handling, or processing is not permitted under HIPAA.
❌ Myth 3: Electronic Access Is Optional
✅ Question #3. Are we obligated to provide electronic copies of PHI if requested by the patient?
✅ Correction #3: Yes. If the PHI is maintained electronically and the patient requests an electronic copy, you must provide it in the requested format if it is readily producible. This includes formats like secure email or through a patient portal.
❌ Myth 4: We Can Deny Access If We Believe It's Not in the Patient's Best Interest
✅ Question #4: Can we withhold information that might upset or confuse the patient?
✅ Correction #4: No. Patients have the right to access their PHI. Denying access based on subjective beliefs about a patient's best interest is not permissible. Denials are only allowed under specific circumstances defined by HIPAA, such as when releasing the information could endanger the life or physical safety of the patient or another person. Even then, proper procedures must be followed, including:
- Providing a written denial that explains the reason for the denial.
- Informing the patient of their right to have the decision reviewed.
- Outlining the process for filing a complaint.
❌ Myth 5: Patients Must Provide a Reason for Their Request
✅ Question #5: Is it acceptable to ask patients why they want access to their medical records?
✅ Correction #5: No. Patients are not required to provide a reason for requesting their PHI. The right to access is unconditional, and providers should not impose additional barriers by requesting justifications. Asking for a reason can be seen as a form of access obstruction and may lead to compliance issues.
The Overlooked Aspect: Information Blocking and Its Implications
While compliance with HIPAA's Right to Access is essential, an often-overlooked dimension is the relationship between HIPAA and the Information Blocking Rule under the 21st Century Cures Act.
Understanding Information Blocking
- Definition: Information blocking refers to practices likely to interfere with, prevent, or materially discourage access to, exchange of, or use of Electronic Health Information (EHI).
- Applicability: Applies to healthcare providers, health IT developers, and health information exchanges.
- Exceptions: The rule outlines specific exceptions where information blocking is permissible, but these are narrowly defined.
Implications for Providers
- Stricter Timeliness Standards: The Information Blocking Rule often demands more immediate access than HIPAA's 30-day requirement. Delays without a valid exception may be considered information blocking.
- Broader Scope of Information: Includes a wider array of EHI beyond what is traditionally defined as PHI under HIPAA.
- Potential Penalties: Non-compliance can result in significant financial penalties and increased scrutiny from regulatory bodies.
Key Point
Failing to provide timely access violates HIPAA and may constitute information blocking, exposing providers to additional enforcement actions and penalties.
Best Practices for Ensuring Compliance

To avoid similar pitfalls and uphold patient rights, healthcare providers should adopt the following strategies:
1. Reviewing/Updating Policies and Procedures
✅ Regular Audits: Periodically assess your organization's policies related to patient access to ensure they align with current laws and regulations.
✅ Policy Updates: Adjust policies promptly in response to changes in regulations or operational practices.
2. Investing in Consistent Staff Training
✅ Comprehensive Training Programs: Educate all staff members involved in handling PHI on HIPAA requirements and the Information Blocking Rule.
✅ Continuous Education: Provide ongoing training to update staff on regulatory changes and best practices.
3. Implementing Efficient Systems and Technology
✅ Electronic Health Records (EHR) Systems: Utilize robust EHR systems that facilitate easy retrieval and secure transmission of electronic PHI.
✅ Patient Portals: Provide patient portals to enable individuals to access their health information directly. Automated Tracking: Use systems to monitor the status of access requests to ensure timely responses.
4. Enhancing Communication Protocols
✅ Prompt Acknowledgment: Confirm receipt of access requests immediately and provide clear information on expected timelines.
✅ Transparent Updates: Inform patients promptly about delays and provide written notices when necessary.
✅ Feedback Mechanisms: Encourage patients to share feedback on the access process to identify areas for improvement.
5. Developing Contingency Plans
✅ Emergency Preparedness: Create plans to maintain critical operations during unforeseen events, ensuring compliance is upheld.
✅ Resource Allocation: Ensure adequate staffing and resources are allocated to handle access requests promptly, even during high-demand periods.
Conclusion
Timely access to health information is a cornerstone of patient-centered care. It empowers individuals to make informed decisions and fosters trust between patients and providers. The HIPAA Right to Access is not merely a regulatory requirement—it's an ethical obligation to support patient autonomy and transparency.
Healthcare organizations must prioritize compliance by understanding the full scope of their responsibilities, including the implications of the Information Blocking Rule. By debunking common myths, learning from real-world cases like the Rio Hondo incident, and implementing proactive strategies, providers can safeguard against violations, protect their reputations, and, most importantly, uphold the rights and well-being of their patients.

